2024 E/M Documentation and Coding Changes
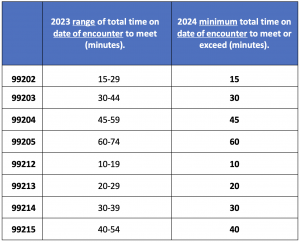
2024 office visit codes 99202-99205 and 99212-99215 are revised to remove the time “range” in minutes from each code. Instead, clinicians billing based on time requires a single “minimum time threshold” to meet or exceed.
AMA CPT is not changing the descriptor to 99211 Office or other outpatient visits for the evaluation and management of an established patient that may not require the presence of a physician or other qualified health care professional. You will continue to bill this code per usual in 2024.
The E/M update includes new guidelines for multiple same-day E/M visits in the hospital and nursing facility settings.
- Per day: The hospital inpatient and observation care services and the nursing facility services are “per day” services. When multiple visits occur over the course of a single calendar date in the same setting, a single service is reported.
- When using MDM for code level selection, use the aggregated MDM over the course of the calendar date. When using time for code level selection, sum the time over the course of the day using the guidelines for reporting time.
Multiple encounters in different settings or facilities
Newly added instructions for reporting hospital inpatient/observation care services and admission and discharge services when a patient stay spans over 2 calendar dates.
A patient may be seen and treated in different facilities (e.g., a hospital-to-hospital transfer). When more than one primary E/M service is reported and time is used to select the code level for either service, only the time spent providing that individual service may be allotted to the code level selected for reporting that service. *No time may be counted twice when reporting more than one E/M service.
The designation of the facility may be defined by licensure or regulation. Transfer from a hospital bed to a nursing facility bed in a hospital with nursing facility beds is considered as two services in two facilities because there is a discharge from one type of designation to another.
Prolonged services are also based on the same allocation and their relationship to the primary service. The designation of the facility may be defined by licensure or regulation.
An intra-facility transfer for a different level of care (e.g., from a routine unit to a critical care unit) does not constitute a new stay, nor does it constitute a transfer to a different facility.
- The nursing facility setting should note the five-minute time increase for 2 visits.
- Initial Nursing Facility Care, 99306 will require 50 minutes total time.
- Subsequent Nursing Facility Care, 99308 will require 20 minutes of total time.
Emergency department (ED) and services in other settings
*same or different facilities
Time spent in an ED by a physician or other QHP who provides subsequent E/M services may be included in calculating total time on the date of the encounter when ED sets are not reported and another E/M service is reported (e.g., hospital inpatient and observation care services).
Discharge services and services in other facilities
Each service may be reported separately if any time spent on the discharge service is not counted towards the total time of a subsequent service in which code level selection for the subsequent service is based on time.
Time includes any hospital inpatient or observation care services (including admission and discharge services) time (99234, 99235, 99236) because these services may be selected based on MDM or time. When these services are reported with another E/M service on the same calendar date, time related to the hospital inpatient or observation care service (including admission and discharge services) may not be used for code selection of the subsequent service.
Discharge services and services in the same facility
If the patient is discharged and readmitted to the same facility on the same calendar date, report a subsequent care service instead of a discharge or initial service. For E/M reporting, this is a single stay.
Discharge services and services in a different facility
If the patient is admitted to another facility, for the purpose of E/M reporting this is considered a different stay. Discharge and initial services may be reported as long as time spent on the discharge service is not counted towards the total time of the subsequent service reported when code level selection is based on time.
Critical care services
*including neonatal intensive care services and pediatric and neonatal critical care.
Reporting guidelines for intensive and critical care services that are performed on the same calendar date as another E/M service are described in the service specific section guidelines.
If the patient is seen in two settings and only one service is reported, the total time on the date of the encounter or the aggregated MDM is used for determining the level of the single reported service.
If prolonged services are reported, use the prolonged services code that is appropriate for the primary service reported, regardless of where the patient was located when the prolonged services time threshold was met. The choice of the primary service is at the discretion of the reporting physician or other QHP.
*Transitions between office or other outpatient, home or residence, or emergency department and hospital inpatient or observation or nursing facility: See the guidelines for Hospital Inpatient and Observation Care Services or Nursing Facility Services.
Split/Shared E/M Updates
The new CPT guidelines adopt the CMS concept of calculating the substantive portion to determine which team member reports the visit for shared/split E/M services.
- “If code selection is based on total time on the date of the encounter, the service is reported by the professional who spent the majority/more than half of the face-to-face or non-face-to-face time performing the service.”
- “For the purpose of reporting E/M services within the context of team-based care, performance of a substantive part of the MDM requires that the physician(s) or other QHP(s) made or approved the management plan for the number and complexity of problems addressed at the encounter and takes responsibility for that plan with its inherent risk of complications and/or morbidity or mortality of patient management. By doing so, a physician or other QHP has performed two of the three elements used in the selection of the code level based on MDM. If a practice codes the visit based on medical decision-making (MDM), the practitioner who performs the problems addressed and risk portions of the visit reports the service.”
Although we make every reasonable effort to assure the accuracy of the information within these pages at the time of publication, the Medicare program is constantly changing, and each provider is responsible for staying informed of the Medicare program requirements. Any regulations, policies and/or guidelines cited in this publication are subject to change without further notice. Current Medicare regulations can be located on the CMS website.