The various image-guided percutaneous procedures used to treat Vertebral Fractures include terms such as Vertebroplasty, Kyphoplasty, Sacroplasty and Augmentation. The nuances of these procedures often cause confusion. This article discusses these procedures, their documentation, and CMS policy to obtain more clarity.
Primary Code Sets
There are three procedure code sets detailed below for:
- Vertebroplasty
- Augmentation/Kyphoplasty
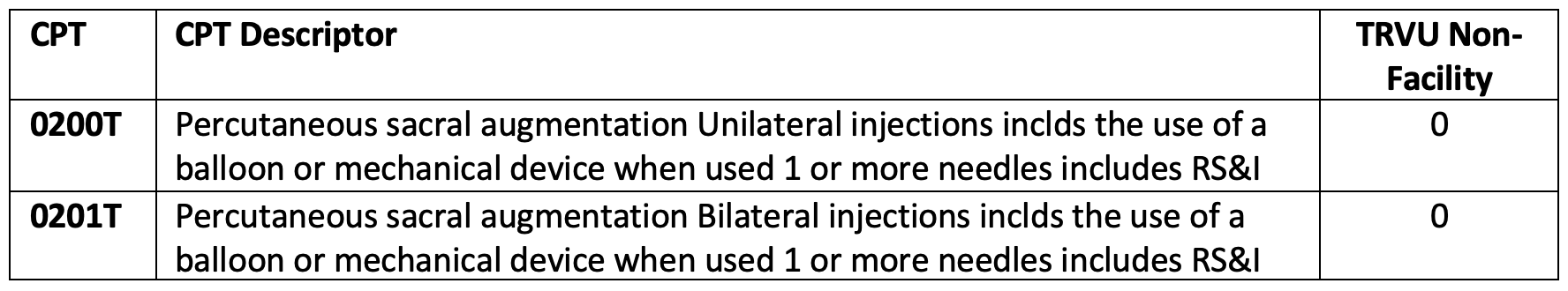
- Augmentation/Sacroplasty
The augmentation codes (22513-22515 & 0200T, 0201T) are often referred to as kyphoplasty, however, the CPT descriptors do not contain this term in the verbiage.
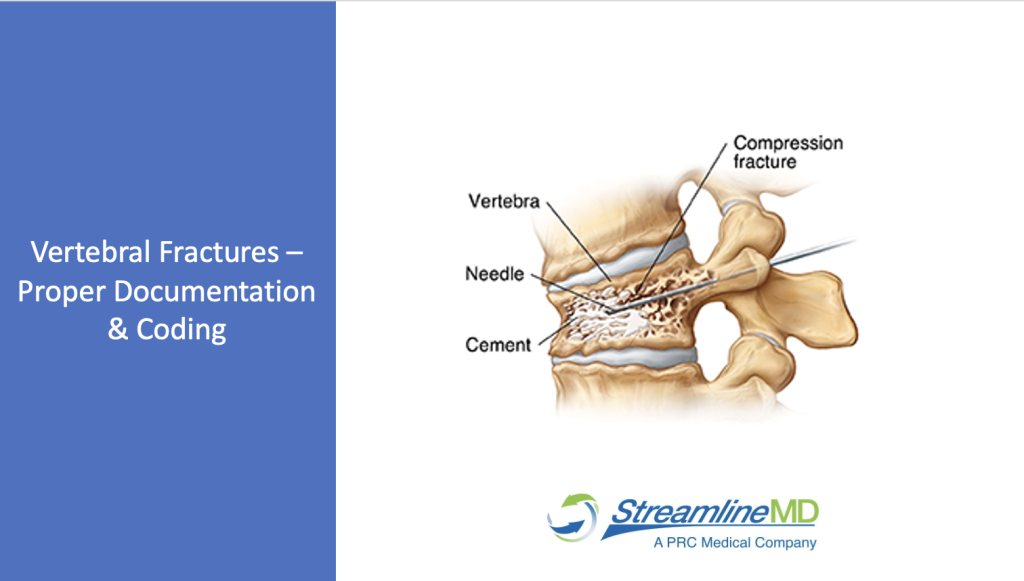
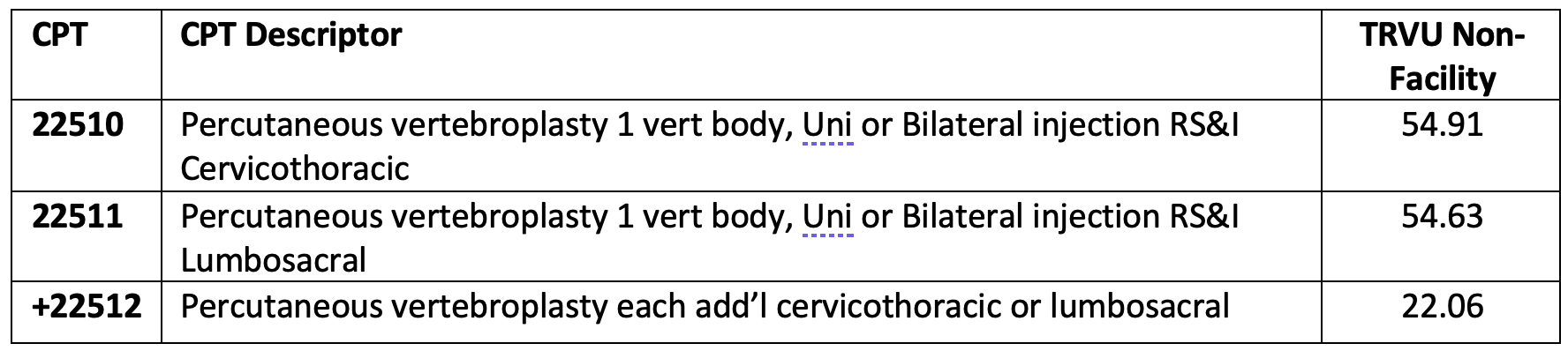
Vertebroplasty
- Replaces vertebral body marrow with cement by injecting cement into a partially collapsed vertebral body.
- Space/cavity/channel is not created during vertebroplasty. When placement of a needle or cannula causes displacement of bony material, this is not an augmentation. It must be an intentional cavity creation to utilize augmentation codes.
- Includes Radiologic Supervision and Interpretation
- Includes bone biopsy when performed.
Augmentation aka Kyphoplasty
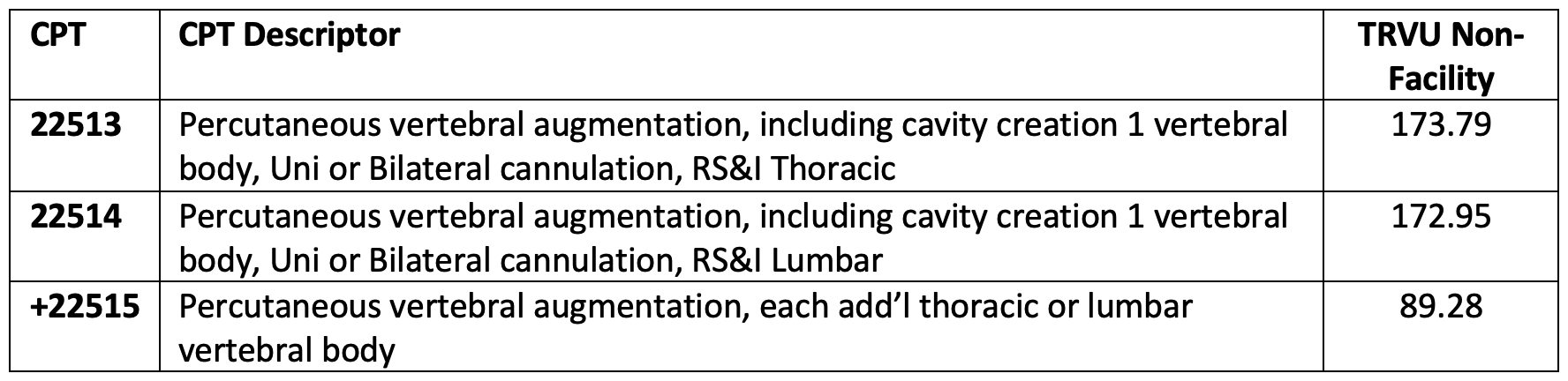
- After creating a cavity with a mechanical device, cement is injected into the cavity and vertebral body to generate expansion of the space to regain lost vertebral height.
- Requires cavity/space/channel creation with mechanical device and injection of cement.
- Creating a space/cavity/channel is required to perform and bill for augmentation.
- Includes Radiologic Supervision and Interpretation
- Includes bone biopsy and fracture reduction when performed.
Sacral Augmentation aka Sacroplasty
- After creating a cavity with a mechanical device, cement is injected into the cavity and vertebral body to create expansion of the space to regain lost vertebral height.
- Requires cavity creation with mechanical device and injection of cement.
- Creating a space/cavity/channel is required to perform augmentation.
- Includes Radiologic Supervision and Interpretation
- Includes bone biopsy when performed.
- Cervical Augmentation/Kyphoplasty, Unlisted CPT 22899
Proper Documentation
Documentation should provide a detailed description of the procedure including the type of imaging guidance used for needle/device/placement.
Oftentimes, providers are unaware that when a balloon is not utilized, but a cavity is created with a curette, etc. this is considered an augmentation and billable with the augmentation code set 22513-22515
Therefore, a thorough description of the mechanical device used for intentional cavity creation is an important component of the interpretation for coders to assign correct code(s). If an experienced coder is unsure of what was performed due to lack of clarity in the report, it is highly unlikely the insurance adjudicator will understand the report which could result in a denial. Consideration of all audience members of the report should be a factor for documentation.
Bone Biopsy is included in both vertebroplasty and augmentation codes and may not be coded separately unless a separate, distinct site from treatment. Augmentation also includes fracture reduction when performed.
Contrast injections performed to evaluate venous drainage are not separately billable.
Clinical Indications
Per Clinical Examples in Radiology, Summer 20:10 if Kyphoplasty and vertebroplasty are performed on different levels during the same session, bill for the Kyphoplasty using 22513 & 22514 and the vertebroplasty utilizing 22510 & 22511. Verify CCI edits and apply modifier(s) as appropriate.
Clinical Indications for this therapeutic treatment are spinal fractures with the goal of pain relief. CMS covers six ICD10 Diagnosis Codes for vertebroplasty and augmentation/kyphoplasty when performed for pathological fractures due to osteoporosis, or neoplasms. CMS does not cover these procedures for traumatic spinal fractures.
Payer Guidelines
CMS NCD for 22510-22512 & 22513-22515
CMS does not cover Sacral Augmentation/Sacroplasty, Category III codes. 0200T & 0201T
Non-covered services for Medicare patients require obtaining and ABN. Be sure to review and follow CMS rules for obtaining an ABN prior to the day of the procedure.
Review managed care policies to confirm coverage for patient’s plan. Managed care carriers require a signed waiver when services are not covered by the patient’s plan. Verify the plan coverage prior to obtaining a waiver before the day of treatment.
Some managed care carriers list the conditions they cover, but not the specific ICD-10 codes, which makes it even more valuable to document the patient’s complete history (e.g., fracture due to…) and include the most specific indications in the report.
Assign internal RVUs for 0200T, 0201T & 22899 based on feedback from the providers as to what this procedure is most similar to for determining the RVUs to be assigned internally for productivity benchmarking.
Conclusion
When all of these factors are taken into consideration prior to the procedure, reimbursement for these procedures should be attainable.
References:
CMS, AMA/ACR Clinical Examples in Radiology, CPT, SIR
StreamlineMD provides EHR & RCM Software & Service imaging & imaging-Guided Procedure Specialists. Our mission is to improve Healthcare for All Americans. Our core values that guide us on our mission are Service Quality, Teamwork, Efficiency, Adaptability, Communication, and Integrity. Learn more about us at StreamlineMD.com.